Virtusa Recognized as Global Leader in Gen AI Services by ISG Provider Lens® - Read report
Lean into data mastery to extend patient-centered care and promote health equity | Read the report
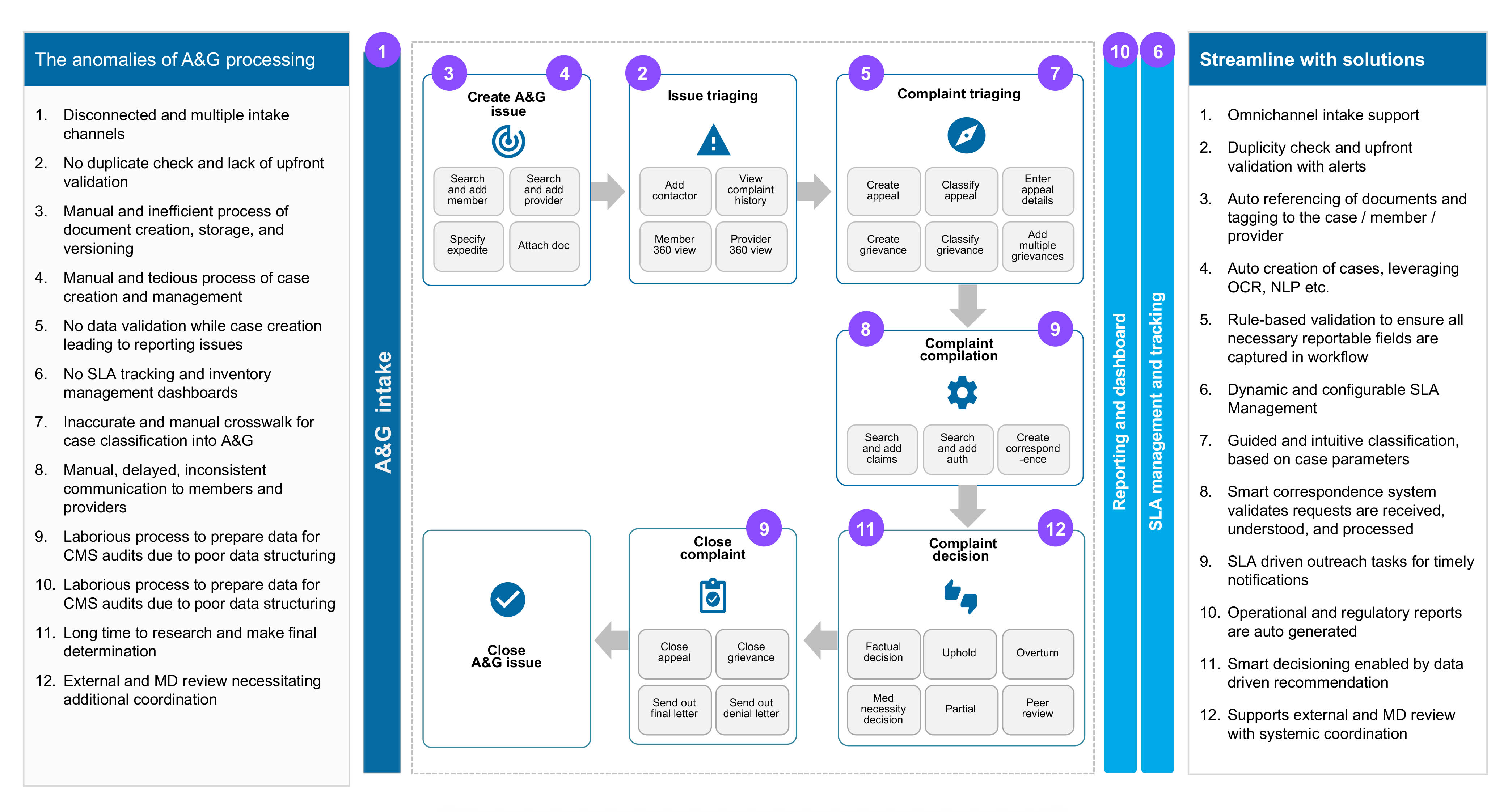
Transforming the appeals & grievances processing
with intelligent digitization
Consulting leader, Healthcare and Life sciences
Member complaints, appeals and grievances (A&G), are one of the most challenging and sensitive business responsibilities that payers must manage. In a highly regulated healthcare industry, providing timely resolutions to members by complying with CMS guidelines and business SLAs can be complex and manual-intensive effort.
In most scenarios, noncompliance to regulations and making quick and accurate decisions in appeals & grievances processing within a prescribed timeline leads to substantial financial penalties. The challenge is to navigate unpredictable workloads and disintegrated data flows across the enterprise.
This is where the payers need to quickly deploy intelligent, automated appeals and grievances process management for real-time insights and monitoring. Payers that are looking to make a differentiated impact must take the right step towards boosting quality scores and successful CMS star rating with digitized A&G processing. It helps to:
- Augment business outcomes with an assured 8-12% boost in CMS star rating
- Achieve 30% operational cost reduction and higher efficiency by shifting to an AI-enabled A&G platform
- Enhance member and provider satisfaction by advancing to an intelligent appeals workflow
Understanding the challenges in the appeals and grievances business
The star rating impacts the customer’s decisions in a competitive marketplace and affects a member’s plan selection. Faster response times enabled by technology has a significant role to play in customer satisfaction. However, technological modernization is not applied uniformly across the enterprise. It leads to capability disparities, broken workflows, and data silos. Heterogeneous tech transformation, along with inefficient processing, leads to noncompliance.
The complexity for healthcare payers increases with multiple federal acts and rules, all of which directly impacts the A&G processing:
- Audit & Appeals Fairness, Integrity and Reforms in Medicare Act (AFIRM)
- Patient Protection and Affordable Care Act (ACA)
- Health Insurance Portability and Accountability Act (HIPAA)
- Social Security Act (SSA)
Business processes also need to provision for reviews by external entities. Payers need to track the event details and decisions at multiple levels. The A&G escalation matrix:
- Appeal Level 1: Org reconsideration
- Appeal Level 2: Independent review entity (IRE)
- Appeal Level 3: Administrative law judge (ALJ) review
- Appeal Level 4: Medicare appeals council (MAC)
- Appeal Level 5: Judicial review by the federal district court
Performance indicators for A&G business
Process efficiency
- Advanced interconnected workflows (HIPAA compliant)
- Unified intake for complaints, appeals, grievances
- Smart decision making with key ops dashboard and metrics
- SLA-driven ability to track, route, and expedite cases
Resolution timeliness
- Ability of real-time tracking of cases
- Effective management of SLAs
- Alerts and notifications against goals and deadlines
- Template-driven uniform and timely outbound communication
Resolution accuracy
- Upfront validation and duplicate check
- Right data at right point of time for decision making
- Decision recommendation based on historical records
- Additional checkpoints on error-prone areas
Regulatory compliance
- Detailed reporting and key metrics tracking functionality
- Compliant processes to generate compliant reports
- Regulatory audit readiness
- Streamlined CMS universe reports
Efficient processes powered by state-of-the-art technologies
Built for agility, A&G solution powered with intelligent technologies enables healthcare organizations to quickly deploy and modify their appeals and grievances processes to address timeline, compliance, accuracy, and efficiency glitches.
Let us explore how to address the key challenges in your appeals and grievances processing and the pertinent solution for each paving the way for a futuristic integrated model:
Boosting member and provider satisfaction with intelligent technologies
The future belongs to the fast. As manual processes and unpredictable workloads slow down healthcare businesses, payers need to quickly deploy intelligent, automated process management for real-time insights and monitoring. An intelligent Appeals and Grievances (A&G) solution with simplified case management and automated task handling can accelerate case resolution, minimize penalties, and increase customer stickiness.
Artificial intelligence
A prominent technology lever that can help reshape the A&G business process and enable significant saving and accuracy is artificial intelligence (AI), complemented by machine learning (ML) for adaptive models and deep learning for predictive models.
Natural language processing
A significant portion of the A&G data is largely based on physical documents that increase manual effort in the A&G process. One of the key segments of AI, natural language processing (NLP), can help streamline the case intake process for A&G in healthcare. Thus, leveraging NLP can significantly uplift the business value and automation in the intake part of the A&G process and beyond by tracking the incoming emails, chats, or contact center inputs.
Robotics Process Automation
Robotics is another leading technology lever that payer organizations have started leveraging to bridge the legacy platform's interim gaps. In the A&G healthcare business, robotic automation acts as a temporary solution to bring data consistency.
Mobile apps and healthbots
The usage of mobile apps for easier communication on hand-held devices with appropriate augmentation of chatbots is a potential booster in the A&G process. For solving the A&G problems of a payer organization, healthbots have a high potential to make communication seamless between multiple parties.
Conclusion: Improve member satisfaction and compliance through digitized A&G processing
With the emergence of new technologies, digital transformation is no more an option but a necessity for every payer in the healthcare domain. To stay nimble in the face of rapid technological advancements, payers must carefully evaluate their business intents and assess what automation technologies must be deployed for their specific A&G business challenges.
Therefore, a solution equipped to deliver intuitive and guided workflows can help users navigate through the complex case lifecycle of an appeal or a grievance. Data validation and embedding key cleansing rules as part of case workflows can provide clean data audits and compliance submission. Leading-edge AI model and predictive ML capabilities can help build a portfolio of lasting, happy members.
An Appeals and Grievances (A&G) solution engineered with simplified case management, automated task handling, and AI-based appropriate classifications can reduce costs, minimize penalties, and ensure adherence to regulatory compliance. It can assist in:
- Increasing timelines by 13%
- Increasing accuracy by 33%
- Increasing productivity by 66%
Payers need to quickly deploy intelligent, automated process management for real-time insights and monitoring and address the archaic, inflexible systems that hurt financially.
Alok Mandal
Vice President & Global Head, Healthcare and Lifesciences
Alok heads the consulting group for the healthcare and life sciences segment in Virtusa. He is an accomplished domain and technology leader with expertise in developing enterprise business solutions focused on Digital-First strategy leveraging digital process automation, integration components, data analytics, AI, and GenAI. He spearheads critical solution initiatives that are implemented in line with industry trends and go-to-market strategies.
Subscribe to keep up-to-date with recent industry developments including industry insights and innovative solution capabilities
Creating scalable processes with strong reporting
Learn more about our Appeals & Grievances Processing solution